|
Forum for Clinical and Surgical Oral Pathology
Case BBOPF 17-2
Dr. Joseph Rinaggio (Rutgers School of Dental Medicine. Newark, NJ. USA) would like your management advise for the following case (the case will be available for comments from July 18-July 25, 2017).
Clinical History
This is a case that one of my surgeon contributors has consulted me on. He is unsure as to how to proceed with this and would appreciate any help or advice that people would have.
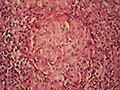
The patient is a 28-year-old female, who works in a high-stress professional job. About 6 months ago, she presented with a diffuse gingival erythema on the mandible and premaxilla that the surgeon described as similar to that of a plasma cell gingivitis. There are no known predisposing factors. A biopsy was performed, which I read out. It was diagnosed as granulomatous inflammation; micro stains were negative, as was polarized light. I suggested that systemic granulomatous disease be ruled out (no other systemic symptoms are present at this time). Crohn's disease has since been ruled out. The patient presented again about two weeks ago with persistent lesions, represented by the first 2 photographs (the two posterior interdental papillae were removed via laser by a general dentist months ago. I don't know why, but they have only recently healed). A biopsy was performed for DIF, which came back negative. The patient was placed on corticosteroids, which she states made the symptoms worse. Since then, small vesicles have appeared (the last picture submitted). Are there any suggestions as to what this might represent, any other tests to order, or how to manage this case?
Joseph Rinaggio, DDS, MS
Images (click for a larger image)





Case prepared by Dr. Alfredo Aguirre (BBOP Manager) and Daniel Emmer (University at Buffalo School of Dental Medicine).
|